Takeaways
- MC4R agonists target the brain’s appetite center to support lasting weight maintenance after initial loss.
- Combining GLP‑1 and MC4R therapies enhances satiety control while minimizing metabolic rebound.
- Fountain of Youth SWFL leads in integrating emerging CNS‑based therapies for personalized weight management.
Targeting the CNS: Why Oral Synergists Are Gaining Ground
New therapies for weight maintenance increasingly focus on the brain’s command center: the central nervous system. Oral CNS synergists activate key neurocircuitry to reduce appetite without relying on gastrointestinal cues. Unlike injectables, they promote lasting changes in hypothalamic signaling that support post-weight-loss maintenance. MC4R agonists work within this model to re-tune satiety thresholds and prevent rebound weight gain. These compounds represent a promising category for long-term success beyond short-term loss strategies.
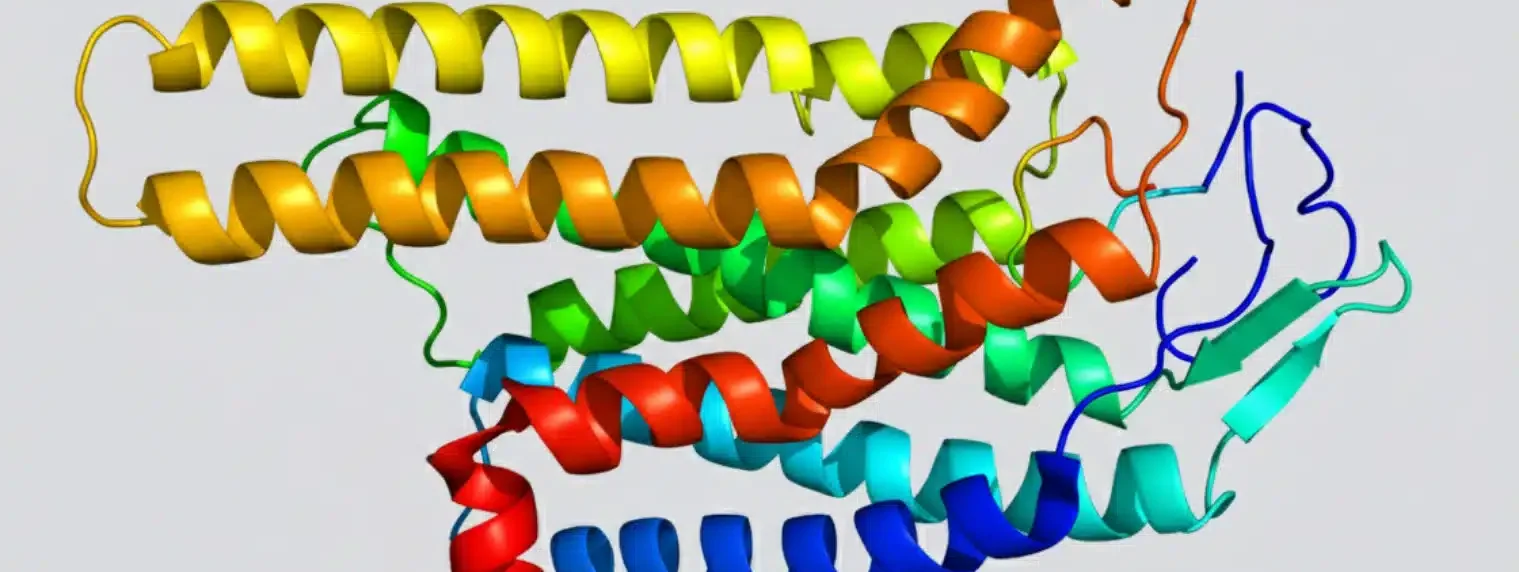
The Melanocortin System and Energy Balance
Hypothalamic Nodes of Appetite Regulation
The hypothalamus regulates hunger using POMC neurons that signal through the melanocortin pathway. These neurons help suppress appetite and raise energy use when activated. Hormones like insulin and leptin feed back into this circuit to keep energy balance stable. In obesity, this feedback becomes disrupted, weakening satiety and promoting overeating. Targeting these pathways can restore homeostasis and reduce drive to consume excess calories. Research published in the National Center for Biotechnology Information (NCBI) details how central nervous system mechanisms govern food intake and energy regulation.
What MC4R Agonists Actually Do
MC4R agonists mimic natural alpha-MSH, a brain-derived signal that promotes fullness. They stimulate specific receptors in the hypothalamus to lower appetite and boost resting metabolism. Importantly, these drugs avoid other melanocortin receptors linked to stress or pigmentation. Researchers continue refining these agents to maximize specificity and clinical benefit. Improved targeting allows for better weight regulation with fewer off-target effects.
How the CNS Complements Peripheral GLP-1 Activity
GLP-1 drugs reduce hunger by acting through the vagus nerve and brainstem, which relay stomach stretch signals. MC4R drugs act higher up, resetting hypothalamic sensitivity to weight changes. When used together, they engage multiple tiers of appetite control. This two-pronged approach supports more consistent results, especially in patients who experience plateaus with GLP-1 monotherapy. CNS-targeted strategies may fill this critical treatment gap.
The Role of Leptin Resistance and Re-sensitization
Obesity often leads to leptin resistance, blunting the brain’s awareness of energy stores. MC4R activation may restore some leptin sensitivity, enhancing satiety regulation. This re-sensitization process can strengthen long-term weight maintenance and help avoid post-treatment rebound. Early trials show encouraging data in this area, especially in those with known leptin pathway disruption. Future work may refine how best to time MC4R agonist use for these effects.
MC4R Agonists in the Pipeline: What to Watch For
Setmelanotide and Its Initial Indications
Setmelanotide gained FDA approval for rare obesity syndromes involving POMC and LEPR mutations. These syndromes involve broken MC4R pathways from birth, making the drug highly effective. A clinical analysis published in PubMed demonstrated significant and durable weight loss in affected individuals. It also helps confirm the validity of the MC4R pathway as a therapeutic target. Broader trials now test its use in common obesity subtypes.
Next-Gen Compounds in Development
Multiple companies are developing oral MC4R agonists with higher selectivity and daily dosing options. These compounds improve upon setmelanotide’s injectable format and receptor cross-reactivity. Early studies show reduced hunger, improved body composition, and better tolerability profiles. Key questions remain about their long-term safety and use outside rare disease groups. Larger trials are underway to evaluate durability, relapse prevention, and real-world outcomes.
Selectivity and Safety: Key to Broader Use
The melanocortin family includes five receptors, each involved in different systems. MC1R affects pigmentation, while MC2R governs adrenal function. Selectivity for MC4R is essential to avoid darkening skin or triggering stress responses. Researchers use advanced molecular modeling to fine-tune agonist structures and avoid off-target effects. New drugs entering phase II trials show promising selectivity with minimal endocrine or pigment disruption.
Pharmacokinetics and Once-Daily Dosing
Improved oral bioavailability allows for once-daily MC4R agonist administration. These formulations simplify use compared to weekly or biweekly injectables. Consistent dosing enhances receptor engagement and supports steady appetite control. Several agents now in trials reach peak levels quickly without inducing tachyphylaxis. Extended half-lives help avoid withdrawal effects and keep neural circuits stable during therapy.
Differentiating Mechanism from Other CNS Drugs
MC4R agonists do not act on dopamine or serotonin systems linked to mood or addiction. Unlike amphetamines or bupropion, they lack stimulant qualities or abuse risk. Their appetite suppression stems from direct hypothalamic signaling instead of neurotransmitter boosts. This unique profile enables safer, longer-term use. It also makes them suitable for patients who fail or cannot tolerate traditional CNS-based weight medications.
Integration with GLP-1 and GIP Therapies: Synergistic Potential
Dual Pathway Activation for Durable Results
GLP-1 receptor agonists slow digestion and reduce food intake by mimicking gut signals. MC4R agonists enhance this effect by shifting the brain’s interpretation of energy status. Used together, these therapies amplify satiety and reduce compensatory hunger. This combination may preserve results after GLP-1 therapy ends. It offers a transition plan instead of abrupt discontinuation.
Use in Maintenance, Not Just Initiation
GLP-1 agents shine in active weight loss but often lack durability post-treatment. MC4R drugs work well during maintenance, helping preserve reduced weight. Their action on hypothalamic setpoints prevents the brain from resetting to a higher weight baseline. Patients can taper off injectables while maintaining control with oral MC4R support. This staged approach may improve overall adherence and long-term outcomes.
Minimizing Gastrointestinal Side Effects
Nausea and vomiting are common with GLP-1 and GIP-based medications. These symptoms lead many to stop treatment early. MC4R agonists avoid the gastrointestinal tract and act only within the brain. Their mechanism does not stimulate vagal pathways, reducing GI burden. This allows more consistent appetite regulation without physical discomfort. Tolerability plays a key role in long-term success.
Impacts on Metabolic Adaptation
After weight loss, the body often slows metabolism and increases hunger to restore fat stores. This phenomenon, known as metabolic adaptation, undermines success. A review in the National Library of Medicine highlights how these adaptations resist weight maintenance. MC4R activation may offset this by raising resting energy expenditure and supporting sympathetic activity. These agents help maintain the caloric deficit achieved during active therapy. Preventing this rebound effect could make maintenance more attainable.
Clinical Scenarios: Who Might Benefit Most
GLP-1 Intolerant or Non-Responders
Some patients cannot tolerate GLP-1 agonists due to persistent GI symptoms or minimal appetite suppression. MC4R drugs provide a mechanistically distinct pathway to achieve similar goals. Their tolerability makes them a candidate for those previously excluded from pharmacologic treatment. Clinicians can offer alternative routes for weight control using CNS-first strategies.
Those at High Risk for Weight Regain
Patients often regain weight after stopping injectables, especially if behavioral support wanes. MC4R agonists can serve as a maintenance bridge during this vulnerable period. Their effects on hypothalamic regulation may reduce the drive to eat and help protect against fat rebound. These patients benefit from long-term stability and neural recalibration.
Individuals with Genetic Obesity Syndromes
Certain rare obesity syndromes involve direct disruption of the MC4R pathway. For these patients, MC4R agonists offer targeted correction rather than general appetite suppression. Genetic testing helps identify suitable candidates for these therapies. Even in polygenic obesity, those with partial pathway dysfunction may respond well. Fountain of Youth SWFL supports diagnostics to guide precise therapy selection.
Post-Menopausal Women with Hypothalamic Changes
Hormonal shifts after menopause alter energy regulation, often increasing visceral fat and appetite. MC4R-targeted drugs may restore hypothalamic sensitivity and support healthier fat distribution. These changes help address stubborn weight issues in older adults. The brain becomes a primary target as estrogen modulation wanes. Tailored therapy in this group supports quality of life.
Long-Term Non-Surgical Weight Management Candidates
Patients unwilling or unable to undergo bariatric surgery need durable non-invasive solutions. CNS-based agents offer scalable weight maintenance without procedural risks. Oral MC4R agonists fit this role well, especially in those seeking daily therapies with low side effect profiles. They expand the toolbox for long-term care beyond short-term interventions.
The following chart compares MC4R agonists with other commonly used long-term weight maintenance agents. It highlights therapeutic focus, delivery method, and side-effect profiles relevant to long-term CNS-based obesity strategies.
| Agent Class | Primary Target | Delivery | Common Side Effects | Best Fit For |
|---|---|---|---|---|
| MC4R Agonists | Hypothalamus (CNS) | Oral (under development), Injectable (approved) | Headache, Injection site pain (injectables) | Post-GLP-1 maintenance or genetic obesity syndromes |
| GLP-1 Agonists | Gut-Brain Axis | Injectable, Oral (limited) | Nausea, Diarrhea, Gastroparesis | Active weight loss with metabolic improvement goals |
| Bupropion-Naltrexone | Dopamine/Opioid Receptors | Oral | Insomnia, Anxiety, Hypertension | Patients needing mood support with appetite regulation |
| Phentermine-Topiramate | Sympathetic Nervous System | Oral | Dry mouth, Insomnia, Paresthesia | Short-term appetite suppression with stimulant effect |
3 Practical Tips for Considering CNS-Targeted Therapies
Confirm Genetic or Hormonal Contributors First
Before initiating CNS-targeted agents, assess for underlying hormonal or genetic factors driving weight retention. These causes often go unnoticed yet significantly impact treatment response. Leptin levels, neuropeptide patterns, and familial obesity histories provide key clues. Using MC4R drugs in these patients aligns with their physiology.
Use MC4R Agonists During GLP-1 Washout
Patients tapering off GLP-1 therapy often experience hunger spikes and rapid weight gain. Introducing MC4R agonists during this period can stabilize appetite and prevent rebound. Staggering the taper with oral CNS support maintains continuity in satiety signaling. This approach encourages smoother transitions and better long-term outcomes.
Monitor for Mood and Sleep Quality
CNS-active drugs can affect sleep and emotional regulation, even without dopaminergic stimulation. Monitor patients for changes in sleep latency, vivid dreams, or mood shifts. While MC4R drugs do not carry stimulant profiles, their neuroregulatory effects warrant clinical attention. Patient feedback ensures early identification of issues.
What Makes These Agents Unique at Fountain of Youth SWFL
Our Fort Myers team carefully follows MC4R research to bring advanced solutions into practical use. At Fountain of Youth SWFL, we personalize weight loss maintenance plans using CNS insights and emerging therapies. We consider your metabolic background, medication history, and tolerance to tailor care. Whether transitioning from GLP-1 or seeking long-term support, we evaluate if MC4R agonists align with your goals.
Questions? Reach out today to explore your options. Call us at 239-355-3294.
Challenges and Future Research Directions
Limited Data on Long-Term Outcomes
Current studies extend six to twelve months, limiting visibility into multi-year success. Researchers aim to gather longitudinal data on real-world durability. Maintenance over three to five years will better inform guidelines. These data will shape reimbursement and care models.
Personalized Dosing and Genetic Screening
Not all patients respond equally to MC4R stimulation. Genetic polymorphisms influence receptor function and downstream effects. Personalized approaches using sequencing or biomarker panels can guide dose selection. Matching drug type to receptor profile may improve results. Fountain of Youth SWFL stays on top of these precision care developments.
Regulatory Hurdles for Non-Rare Obesity Indications
MC4R agonists currently hold FDA approval only for rare genetic syndromes. Expanding their use to general obesity depends on broader trial data. Approval timelines depend on cardiovascular safety, real-world tolerability, and clinical benefit. Ongoing studies may open access in coming years.
Combining with Other CNS or Endocrine Agents
Combinations with bupropion, metformin, or estradiol remain untested in large trials. These agents may complement MC4R action but pose unknown safety risks. Researchers must define interaction profiles and optimal sequencing. Guidelines will evolve as data accumulates.
Building Real-World Protocols
Weight maintenance protocols often lack structure post-injection. Integrating MC4R drugs into step-down plans requires standardization. Clinics need real-world evidence on timing, monitoring, and taper strategies. The National Institutes of Health emphasizes structured maintenance programs as key to preventing relapse. Fountain of Youth SWFL helps bridge this gap with practical, protocol-driven care.
Frequently Asked Questions
Are MC4R agonists FDA-approved for general obesity?
They are currently approved only for rare genetic syndromes, but broader applications are under investigation.
Can I use MC4R agonists with semaglutide or tirzepatide?
These agents may complement each other. Providers often stagger them to reduce withdrawal effects during transition.
Do MC4R agonists cause the same nausea as GLP-1 drugs?
No. Their mechanism avoids gut involvement, resulting in much lower rates of gastrointestinal symptoms.
Are there oral forms available yet?
Yes. Most pipeline candidates use oral formulations designed for once-daily use.
Who should not use MC4R agonists?
Patients with adrenal disease or severe psychiatric conditions may not be appropriate candidates. Screening is essential.
Ready to protect your results after GLP-1? Call our expert team at 239-355-3294 to explore tailored maintenance plans using the latest CNS strategies.
Medical review: Reviewed by Dr. Keith Lafferty MD, Medical Director at Fountain of Youth SWFL on November 1, 2025. Fact-checked against government and academic sources; see in-text citations. This page follows our Medical Review & Sourcing Policy and undergoes updates at least every six months. Last updated November 1, 2025.