Takeaways
- Wearable nanobiosensors offer real-time hormone tracking through sweat or interstitial fluid.
- Closed-loop adaptive systems adjust HRT dosing based on live feedback instead of static lab tests.
- These technologies enhance precision and safety for menopause, perimenopause, and testosterone support.
From Trial-and-Error to Targeted Precision
Hormone Replacement Therapy (HRT) often walks a fine line between benefit and risk. Dosages must account for metabolic differences, receptor sensitivity, and fluctuating endogenous levels. Historically, even in bioidentical HRT protocols, personalization depended on intermittent lab testing and patient feedback. Wearable nanobiosensors are now changing this by enabling real-time hormone tracking, pushing hormone care into an adaptive, closed-loop model.
This shift mirrors transformations already underway in diabetes care, where continuous glucose monitors (CGMs) allow real-time insulin titration. But in HRT, where microgram shifts in estradiol, progesterone, or testosterone can impact mood, cognition, and cancer risk, adaptive technology holds an even greater promise.
At Fountain of Youth in Fort Myers, we stay at the forefront of these emerging innovations by closely monitoring advancements in sensor-integrated care models and precision dosing systems.
How Nanobiosensors Monitor Endocrine Signals in Real Time
Core Mechanisms Behind Hormone Detection
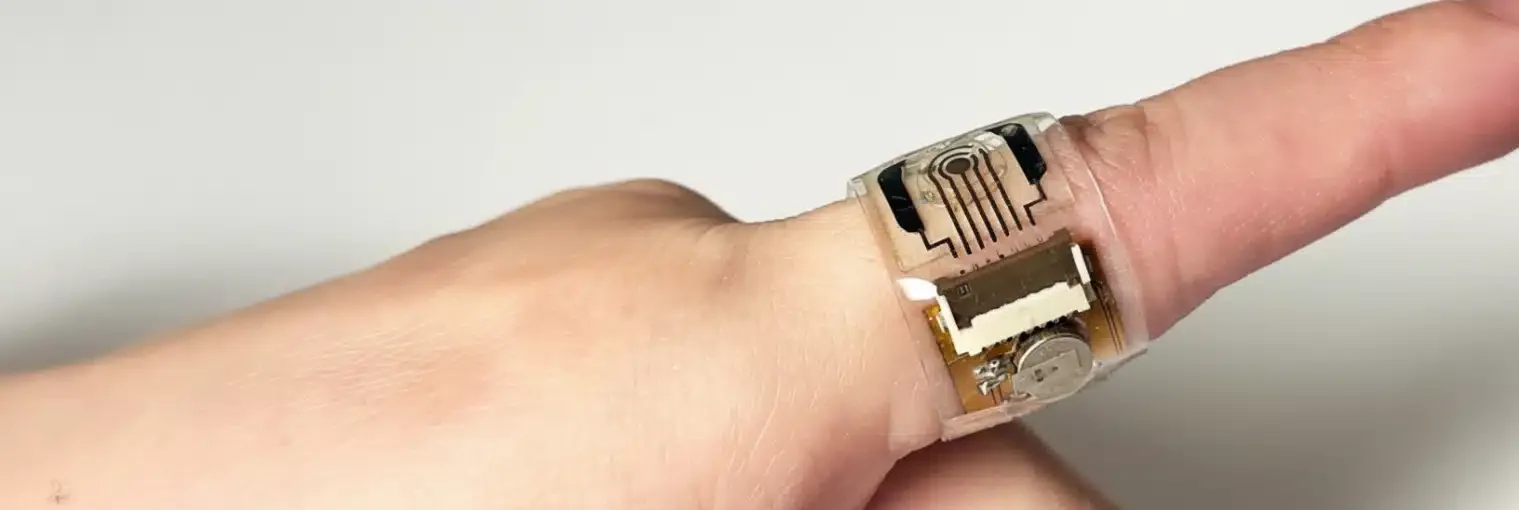
Nanobiosensors are engineered to detect molecular changes in sweat, interstitial fluid, or blood using miniaturized biorecognition elements. Antibodies or aptamers bind specifically to hormones such as estradiol or progesterone, triggering electrical or optical changes read by a processor. This allows near-continuous hormonal tracking at the skin level, as demonstrated in wearable biosensor platforms for hormone detection.
Sweat and Interstitial Fluid as Sampling Mediums
Unlike traditional serum sampling, these sensors often use sweat or interstitial fluid, minimizing invasiveness. Microfluidic platforms collect and filter trace hormones, while embedded processors convert those readings into quantifiable levels. Although still in development, multi-hormone wearable patches show strong correlation with plasma values in early trials.
Integration with Smartphones and Cloud Analytics
Most nanobiosensor systems link to mobile apps that interpret and visualize the data. This allows patients and clinicians to monitor hormonal fluctuations in real-time, uncovering patterns tied to circadian rhythm, sleep, stress, and medication timing.
Adaptive Dosing: From Static Protocols to Dynamic Feedback Loops
Feedback Algorithms Tailored to the Endocrine System
Once a wearable device establishes a baseline hormonal rhythm, it can recognize anomalies or trending drops and elevations. The data feeds algorithms trained to adjust dosing schedules, delivery method, or compound strength in response to minute shifts. This adaptive dosing can occur as alerts to prescribers or pre-programmed titration in automated systems.
Closed-Loop Systems with Drug-Delivery Integration
Next-generation platforms merge sensing and delivery into a single wearable. Micropumps or iontophoresis patches release calibrated hormone doses in real-time based on detected levels. This resembles insulin pump systems but requires tighter control due to the narrow therapeutic index of sex steroids.
Personalized Pattern Recognition and Cycle Optimization
For women undergoing HRT after hysterectomy or menopause, nanobiosensors help map residual cycle-like patterns or circadian hormone rhythm. Adaptive dosing systems can then sync hormone release with optimal biological windows for cognition, sleep, and bone remodeling.
Clinical Use Cases That Show Promise
Menopausal Symptom Fluctuations
Patients often report hot flashes, insomnia, or mood changes at seemingly random times. Wearables help correlate symptoms with hormonal dips, allowing personalized schedule adjustments instead of monthly dosage increases.
Perimenopause Hormone Chaos
During perimenopause, hormone levels fluctuate dramatically from day to day. Real-time sensing enables shorter-term predictions and response dosing for patients who don’t fit traditional protocol timing.
Post-Hysterectomy Estrogen Monotherapy
In patients without a uterus, estradiol monotherapy must remain tightly balanced. Wearables can detect unexpected dips that may increase cardiovascular risk or surges that increase breast tissue density, prompting micro-adjustments.
Testosterone Support in Midlife Men
Precision endocrinology also benefits men undergoing testosterone replacement. Nanobiosensors can identify aromatization surges, flagging conversion to estradiol. This allows earlier dose or compound changes to prevent side effects like gynecomastia.
Cancer Survivors in Hormone-Sensitive Recovery
Women with BRCA mutations or hormone-receptor-positive cancer histories may still require symptom relief. Wearable biosensors allow ultra-low-dose HRT titration with better risk surveillance over time.
Challenges Still Facing Closed-Loop Hormone Dosing
Sensor Sensitivity and Specificity
Unlike glucose or oxygen, sex hormones occur in low picomolar concentrations. Sensors must distinguish minute estradiol levels from similar steroid compounds, which remains a hurdle in commercial development.
Skin Compatibility and Signal Interference
Sweat-based sensors must work through skin oil, friction, and variable hydration. Ensuring consistent readings in humid climates like Florida poses design and material challenges for wearables.
Regulatory and Clinical Trial Barriers
FDA clearance for wearable hormone monitors will require longitudinal safety and efficacy studies. Ongoing studies, such as Clinical Trial NCT06980753, aim to validate continuous steroid monitoring in real-life conditions.
Cost and Reimbursement Limitations
Insurance coverage for adaptive hormone tech still lags behind metabolic counterparts like CGMs. Until broader payer adoption occurs, clinics may need to offer concierge models or integrate these tools into existing cash-pay HRT programs.
Patient Education and Trust in Algorithms
Some patients may resist algorithm-driven care without strong provider guidance. Clinicians must educate patients on how adaptive systems enhance safety and personal control rather than remove the human element.
How Precision Endocrinology May Redefine HRT Protocols
Smaller Starting Doses, Titrated Up Dynamically
Instead of starting with a fixed dose and adjusting monthly, clinicians could initiate ultra-low protocols that titrate automatically in response to real-time feedback. This reduces risk of overdose symptoms during the ramp-up phase.
Better Morning-Afternoon Dosing Splits
Wearable feedback allows providers to map diurnal variations and match split-dosing protocols to energy, mood, and sleep cycles. For example, estradiol transdermal microdosing may peak mid-day while progesterone peaks in the evening to aid sleep.
Reduction in Side Effects and Overcorrection
Many HRT side effects stem from overcorrection or delayed dose response. Adaptive systems can prevent wide hormonal swings by smoothing dosing transitions, particularly during sensitive phases like early menopause.
Integration into Post-COVID Metabolic Syndrome Protocols
Post-COVID endocrine disruption has triggered rising interest in wearable hormone support. Precision endocrinology may soon integrate with metabolic trackers to align hormonal and inflammatory data in recovery protocols.
A Future of Hormone Care as Daily Self-Tuning
The ultimate promise lies in making hormone balance a daily, self-adjusting parameter—like hydration or blood sugar. With real-time feedback and guided AI support, patients regain agency over aging and vitality.
Questions? We’re happy to explain how personalized hormone care works at our clinic. Give us a call at 239-355-3294 and speak with our HRT experts today.
The chart below compares conventional hormone monitoring strategies with sensor-based adaptive systems. It highlights key differences in dosing precision, symptom response time, and lab dependency.
| Feature | Traditional HRT Monitoring | Adaptive HRT with Nanobiosensors |
|---|---|---|
| Dosing Adjustment Frequency | Monthly or quarterly, based on static labs | Daily to weekly, based on real-time sensor feedback |
| Lab Dependency | High — requires serum testing every few months | Low — continuous monitoring via interstitial fluid or sweat |
| Personalization Level | Limited to prescriber’s interpretation of periodic lab values | Dynamic — algorithms respond to real-time trends and fluctuations |
| Response Time to Symptoms | Delayed — often weeks between symptom report and protocol change | Rapid — symptoms can be correlated with same-day hormonal changes |
3 Practical Tips for Patients Considering Adaptive HRT
Start Tracking Symptoms Digitally Before Using Wearables
Begin with a journal or app to log daily symptoms, energy levels, and cycle patterns. This gives context when transitioning to sensor-guided care.
Choose Providers Who Understand Hormone Microdosing
Not all clinics tailor doses as tightly as needed for closed-loop protocols. Look for clinicians experienced in microtitration and wearable integration.
Focus on Consistency for Reliable Sensor Readings
For those using wearables, applying sensors at the same time daily and avoiding heavy sweating during readings helps maintain data quality.
What Sets Our Approach Apart
At Fountain of Youth SWFL, we work with advanced diagnostic platforms and continuously monitor research in the wearable HRT space. Our care team understands that precision dosing isn’t just about technology—it’s about connecting data to how you feel each day.
Whether you’re transitioning into menopause, navigating surgical hormone loss, or seeking bioidentical optimization, our protocols evolve alongside these technologies, including newly published findings like wearable hormone monitors for fertility and menopause.
Questions about how this could fit your lifestyle? We’re here to guide you. Give us a call at 239-355-3294 to learn more about your options.
Frequently Asked Questions
Can these sensors replace blood work entirely?
Not yet. While wearables offer daily insights, confirmatory lab work remains essential for calibration and long-term safety monitoring.
Are these devices FDA approved?
Some early-stage platforms are in trials, but most are still considered investigational. We track each product’s clinical progression closely.
Is this technology safe for hormone-sensitive cancer survivors?
Low-dose, feedback-guided protocols may offer symptom control with less systemic exposure, but every case requires oncologist approval.
Can men use these sensors for testosterone therapy?
Yes. Emerging devices detect testosterone and estradiol, helping male patients avoid dosing errors and side effects like mood swings.
Do you offer these wearable systems at your Fort Myers clinic?
We evaluate each new technology based on safety, performance, and patient fit. Ask our team which tools may be suitable for you, or review data like the immunologic impact of hormone loss to guide your questions.
Medical review: Reviewed by Dr. Keith Lafferty MD, Fort Myers on November 1, 2025. Fact-checked against government and academic sources; see in-text citations. This page follows our Medical Review & Sourcing Policy and undergoes updates at least every six months.