Takeaways
-
Controlled mitochondrial uncouplers like HU6 are in early human trials and show promise for reducing liver fat and body adiposity while preserving lean mass.
-
Organ-targeted and prodrug delivery systems enhance safety by minimizing systemic exposure and mitigating risks historically associated with agents like DNP.
-
Preclinical candidates such as BAM15, CZ5, and OPC‑163493 demonstrate robust metabolic benefits, though only HU6 has advanced to human testing so far.
Why This Matters Now
The surge in obesity rates has pushed scientists to seek non-stimulant therapies that promote fat loss without compromising safety. Traditional treatments often rely on appetite suppression or stimulant-driven thermogenesis, which come with risks of cardiovascular strain. Mitochondrial uncouplers offer a radically different approach by increasing the body’s energy expenditure at a cellular level. These agents trigger fat-burning mechanisms without stimulating the central nervous system. With early human trials now underway, the clinical potential of uncouplers has moved from theoretical to tangible. At Fountain of Youth SWFL, our team remains informed about emerging technologies like this. Our ongoing research reviews and internal case study discussions ensure we stay prepared to support clients as new medical weight loss therapies evolve.
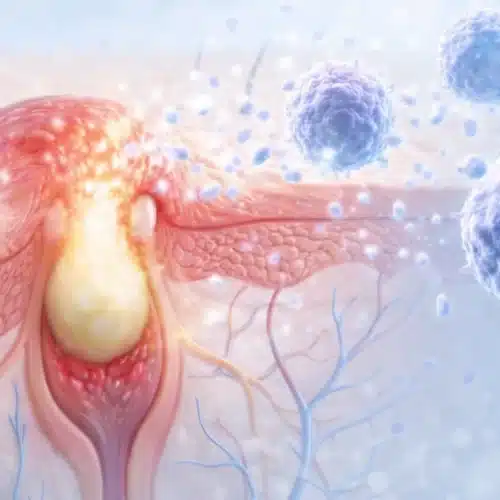
What Are Mitochondrial Uncouplers?
Mitochondrial uncouplers disrupt the standard conversion of nutrients into cellular energy, creating controlled inefficiency. Instead of generating ATP, the energy dissipates as heat, forcing the body to burn more fuel, including stored fat. This metabolic override can significantly boost energy expenditure, especially in fat-dense tissues like the liver. Unlike stimulant-based fat burners, uncouplers do not rely on hormonal pathways or appetite suppression. They act directly within mitochondria, the cell’s energy factories, and enhance thermogenesis. This mechanism can work independently of diet or exercise, though combining them yields optimal results. Early uncoupler research showed impressive effects on obesity markers, including fat mass, insulin sensitivity, and liver function. Yet without precision targeting, these compounds caused severe side effects, leading to regulatory bans.
A Brief (and Controversial) History
The early use of 2,4-dinitrophenol (DNP) in the 1930s demonstrated dramatic weight loss but carried lethal risks. DNP operated as an uncoupler, accelerating metabolism but causing uncontrolled heat production and organ failure. Its ban set the tone for decades of caution. Research into mitochondrial uncoupling didn’t stop but shifted toward understanding how to control the effect safely. Investigators explored targeting uncoupling agents to specific tissues like the liver while avoiding toxicity in muscles or the brain. The goal was to retain metabolic benefits without exposing users to life-threatening hyperthermia. The stigma surrounding DNP delayed mainstream research into therapeutic uncoupling for nearly a century. Only now, with improved drug delivery systems, have researchers revisited the concept with a fresh lens and modern safety protocols.
Breakthroughs in Drug Design and Delivery
Modern mitochondrial uncouplers employ sophisticated drug delivery technologies that drastically lower the risk of systemic toxicity. HU6, the most advanced compound in clinical trials, uses a prodrug design that activates primarily in the liver. This method prevents high peak plasma levels, avoiding the thermal dysregulation that plagued earlier agents. Organ-targeted delivery helps isolate the uncoupling effect to fatty tissue or liver cells, where it’s most needed. Innovations like liposomal encapsulation, nanoparticle transport, and controlled-release coatings further minimize unintended exposure. These breakthroughs have also enabled more accurate dosing, helping researchers find the narrow window where benefits outweigh risks. The result is a generation of compounds that behave predictably and safely in humans—a pivotal change.
Delivery Technologies for Mitochondrial Uncouplers
This chart compares various delivery systems used in current or emerging mitochondrial uncoupler therapies. Understanding their benefits helps clarify how modern science addresses safety and precision in metabolic treatments.
| Delivery Mechanism | Description | Organ Targeting | Safety Advantage |
|---|---|---|---|
| Liver-Activated Prodrugs (e.g., HU6) | Inactive form converted to active drug by liver enzymes | High (liver-specific) | Minimizes systemic exposure and off-target effects |
| Liposomal Encapsulation | Drug encased in fat-like vesicles for controlled release | Moderate (tissue-dependent) | Improves stability and reduces immune activation |
| Nanoformulations | Ultra-small particles engineered for precision targeting | Customizable (high targeting potential) | Reduces dose frequency and improves uptake |
| Sustained-Release Coatings | Time-release polymers control drug release over hours | Low (broad systemic delivery) | Avoids peaks in blood concentration, reducing toxicity risk |
Inside the Human Trials (2024–2025)
Rivus Pharmaceuticals launched Phase 2a and 2b trials to evaluate HU6 in humans with obesity, NAFLD, and heart failure with preserved ejection fraction (HFpEF). In these studies, participants took HU6 daily for eight to nineteen weeks depending on the trial. Results from the NAFLD arm revealed a 33% average reduction in liver fat and meaningful overall fat loss. Participants maintained lean body mass, an outcome that sets HU6 apart from many weight-loss agents. Importantly, no severe side effects were reported during the trial window. Another Phase 2a trial studied the drug in people with obesity-related HFpEF. Here, the compound not only reduced weight but improved cardiovascular fitness and inflammation markers. The follow-up Phase 2b trial, now underway, aims to confirm these effects at a larger scale.
Comparing HU6 to Other Candidates in Development
Other mitochondrial uncouplers like BAM15, CZ5, and OPC-163493 remain in preclinical testing. BAM15 shows potent fat-burning properties in rodents and preserves lean mass while improving insulin sensitivity. CZ5 has yielded similar results but raised toxicity concerns at higher doses. OPC-163493 has shown promising results in liver targeting and metabolic modulation, especially in diabetic mouse models. None of these agents have yet entered human trials due to lingering safety uncertainties. HU6 leads the pack not just because it reached human testing first, but because of its dual impact on liver fat and cardiometabolic risk. If ongoing trials confirm its safety, HU6 could establish the therapeutic blueprint for others.
Target Organs, Safety Windows, and Systemic Impact
Targeting specific organs is crucial to reducing the risk of side effects from mitochondrial uncouplers. The liver plays a central role in lipid metabolism, making it an ideal target for uncoupling activity. By localizing the effect to hepatocytes, drugs like HU6 can maximize fat oxidation while sparing skeletal muscles and other sensitive tissues. This specificity also expands the therapeutic window. Earlier uncouplers had narrow dosage ranges where benefits could turn quickly into risks. HU6’s pharmacokinetics show stable plasma concentrations and minimal systemic spike, which allows researchers to dose with greater confidence. Minimizing oxidative stress and thermogenic overload remains a key safety metric. Trials now include real-time metabolic monitoring to track shifts in heat production, oxygen consumption, and mitochondrial integrity.
Potential Use Cases Beyond Weight Loss
Although marketed primarily as a fat-loss agent, HU6 and similar compounds may benefit several metabolic conditions. In NAFLD and metabolic dysfunction-associated steatohepatitis (MASH), uncoupling reduces intrahepatic lipid accumulation and oxidative damage. Preclinical data also supports uncouplers in reversing insulin resistance, improving blood glucose control, and reducing triglyceride levels. These effects may extend to type 2 diabetes prevention or management. Cardiologists have expressed interest in uncouplers for reducing systemic inflammation and improving vascular function. The HFpEF trial results suggest a broader cardiometabolic impact beyond pure fat loss. Some patients may also benefit from adjunctive therapies like vitamin injections to support energy balance and recovery.
The Regulatory Roadblocks and Safety Hurdles
Despite promising early results, mitochondrial uncouplers face intense scrutiny from regulators. The FDA requires multi-phase safety data that clearly distinguishes controlled compounds like HU6 from illicit DNP analogs. Manufacturers must show not just fat loss but long-term safety, metabolic stability, and minimal risk of misuse. Trials need to demonstrate reversibility, dose tapering, and no rebound effects post-treatment. Ethical concerns also remain. Since uncouplers alter fundamental cellular processes, they must be evaluated not just for efficacy but for bioenergetic consequences in organs that depend heavily on ATP.
3 Practical Tips for Evaluating Emerging Fat-Loss Treatments
- Check for clinical trial participation. Treatments should have transparent human data published in peer-reviewed sources.
- Understand mechanism-based risk. Therapies that manipulate cellular respiration must show clear dose control and tissue targeting.
- Avoid gray-market DNP analogs. Unregulated compounds can be fatal and differ vastly from pharma-grade uncouplers in formulation and effect.
Frequently Asked Questions
What makes HU6 different from DNP?
HU6 is a liver-targeted prodrug with controlled dosing and a wider safety margin. DNP had no organ targeting and caused systemic toxicity. Can mitochondrial uncouplers be used alongside GLP-1 agonists?
Researchers are beginning to explore combination therapies, but no official data exists yet. Always consult with a qualified provider. How fast do results appear in human trials?
In the HU6 trials, measurable reductions in liver fat and body weight occurred within 8 weeks. Are these therapies appropriate for older adults or menopausal women?
Ongoing studies include postmenopausal participants. Many women already exploring hormone replacement therapy may also find uncoupler-based options worth discussing with their provider.
Expert Opinions and Industry Buzz
Obesity researchers at leading conferences have highlighted HU6 as one of the most promising non-stimulant fat-loss interventions. Metabolic medicine panels point to mitochondrial targeting as a foundational shift in treatment philosophy. Industry analysts forecast increasing investment in mitochondrial therapeutics, with a focus on safer delivery systems. Regulatory experts remain cautiously optimistic but emphasize the need for longitudinal data before approval. At Fountain of Youth SWFL, we track these updates closely to provide well-informed options for our clients as new therapies emerge. For those seeking next-level support during weight loss programs, our luxury IV drips provide a premium infusion experience tailored for recovery and energy.
What’s Next in the Fat-Loss Pipeline
The next 12 to 18 months will be critical as Phase 2b trial data for HU6 becomes public. These findings will determine whether HU6 advances to Phase 3, which could include broader patient groups and longer treatment periods. Simultaneously, other uncouplers like BAM15 and CZ5 may progress into early-stage human testing. Researchers also investigate combinations with brown fat activators or GLP-1 agonists to enhance fat-loss synergy. Innovation continues around mitochondrial biogenesis, AMPK modulation, and uncoupling proteins. These adjunct approaches could amplify uncoupler safety and efficiency. Questions? We are here to help! Give us a call at 239-355-3294 to learn how metabolic innovations may fit into your personalized health plan.
Why the Mitochondria Could Redefine Metabolic Medicine
Uncoupling represents more than a new way to burn fat. It reflects a deeper understanding of cellular metabolism and energy control. Rather than suppressing hunger or blocking absorption, uncouplers reshape how cells process fuel. This approach opens pathways for disease prevention, early intervention, and personalized health strategies. As the field matures, mitochondrial modulation may become a cornerstone of metabolic medicine. We believe in staying ahead of that curve—so you can benefit first from what science proves to work.
This article has been reviewed for accuracy by licensed Fountain of Youth SWFL clinicians specializing in mitochondrial‑based weight loss therapies.
Medical review: Reviewed by Dr. Keith Lafferty MD, Fort Myers on September 5, 2025. Fact-checked against government and academic sources; see in-text citations. This page follows our Medical Review & Sourcing Policy and undergoes updates at least every six months.