Takeaways
-
Dual‑pathway therapies deliver stronger, longer-lasting fat loss while preserving lean mass.
-
AI‑guided dosing promises smarter personalization, improving adherence and real‑world outcomes.
-
The oral and injectable co‑agonist amycretin marks a breakthrough in obesity treatment innovation.
The Science Behind Dual-Pathway Therapy
How GLP-1 Works—Suppressing Appetite and Delaying Emptying
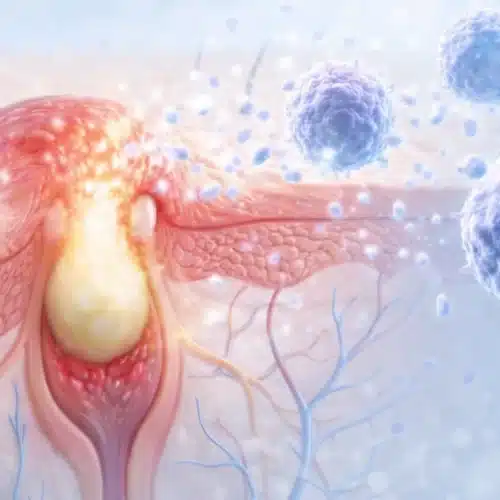
Researchers classify GLP-1 as an incretin hormone that rises rapidly after meals. It promotes insulin secretion while lowering glucagon, thereby smoothing blood glucose swings. The peptide also slows gastric emptying, so fullness lasts longer and appetite drops. Brainstem signals reinforce satiety, which helps people resist high calorie snacks. Because GLP-1 acts quickly, once-weekly analogs maintain stable exposure with minimal daily effort.
Amylin’s Role—Satiety, Energy Regulation, and Metabolic Advantage
Amylin releases alongside insulin from pancreatic beta cells after nutrient intake. It signals the area postrema to slow gastric motility and curb post-prandial cravings. Amylin also decreases glucagon and supports steady hepatic glucose output during fasting. Rodent studies demonstrate increased energy expenditure when amylin signaling remains elevated. Therefore combining amylin with GLP-1 balances appetite suppression with metabolic rate protection.
Why Combining Them Outperforms Single-Hormone Therapy
Dual-pathway therapy targets distinct yet complementary neural and endocrine circuits controlling weight. GLP-1 reduces caloric intake, while amylin maintains higher resting energy expenditure. Clinical data show additive effects, meaning patients lose more fat without extra muscle loss. Consequently physicians anticipate better long-term adherence because hunger rebounds stay minimal. Weight reduction also arrives faster, which encourages motivation during the sensitive early weeks. This synergy explains industry momentum toward co-agonist molecules and combination injectables.
Amycretin: The First Unimolecular GLP-1 + Amylin Co-Agonist
Amycretin trial data reported average weight loss of twenty-four percent over thirty-six weeks with injectable formulation. The oral version demonstrated thirteen percent loss within twelve weeks, offering hope for needle-free treatment. Gastrointestinal symptoms remained mild, and no severe hypoglycemic events surfaced during trials. Novo investigators will launch Phase 3 programs in early twenty-twenty-six across multiple continents. Medical weight loss programs may integrate amycretin pending approval to expand therapeutic options.

Dual hormones and AI reshape weight loss: More fat loss, fewer plateaus, smarter dosing.
Cagrilintide + Semaglutide Combinations in Early Trials
Researchers evaluated weekly cagrilintide paired with semaglutide under the REDEFINE program. Participants achieved roughly twenty percent weight loss after sixty-eight weeks, eclipsing semaglutide alone. Importantly, dual therapy preserved lean mass better than monotherapy which enhances metabolic health. Satiety scores improved quickly, leading to lower dropout rates and sustained adherence. Clinicians note gastrointestinal side effects mirror GLP-1 experience and rarely necessitate discontinuation. These outcomes reinforce the clinical potential of combining separate amylin and GLP-1 analogs before amycretin arrives.
AI-Enhanced Dosing: Pioneering Personalization in Therapy
Clinical Impulses from Diabetes: AI-Driven Dual-Hormone Models
NIH-funded models applied predictive control algorithms to dual-hormone insulin and pramlintide pumps. The system adjusted delivery every five minutes, maintaining glucose within target ninety-one percent of the day. Time-in-range outcomes surpassed single hormone loops by nearly thirty percentage points. These results confirm AI can manage two peptides safely and efficiently in real time. Consequently obesity researchers adopted similar architectures for GLP-1 and amylin dosage simulations.
Translating AI into Obesity Therapy: What’s Possible?
Future algorithms will pull data from wearables, meal logs, and gut hormone assays. The model will forecast hunger peaks, then adjust dual-hormone micro-doses to smooth cravings. Physicians will set safety ceilings, while AI handles day-to-day optimization. Patients may receive weekly reports summarizing calorie trends, weight trajectory, and dosage adjustments. Our Men’s Clinic TRT team already pilots similar data dashboards for lifestyle patients. Questions about this topic? We can help! Give us a call at 239-355-3294 .
Below, the table presents real-world adherence and weight plateau timelines for GLP‑1 monotherapy versus dual-pathway approaches like amycretin. Clear comparison of these outcomes will help patients and clinicians weigh practical long-term sustainability.
Below is a comparison of real-world adherence rates and onset-to-plateau timelines for different weight-loss therapies:
| Therapy Type | Real‑World Adherence | Time to Weight‑Loss Plateau | Key Insight |
|---|---|---|---|
| GLP‑1 Monotherapy | < 50% continue therapy beyond 12 months in real-world | Plateau often occurs around 20 weeks | High dropout, limited sustainability |
| Amycretin (Dual‑Pathway) | Adherence data emerging but encouraging in early trials | Weight‑loss plateau delayed beyond 12 weeks | Promising durability in pilot studies |
| Cagrilintide + Semaglutide | Clinical settings show improved persistence vs monotherapy | Plateau occurs later, weight loss sustained beyond 68 weeks | Stronger motivation and outcomes |
| AI‑Guided Dosing Models | Model systems show ≤10% lapse in control intervals | AI maintains optimal dosing, averting plateau | Adaptive dosing improves long-term outcomes |
What Early Results Reveal: Efficacy, Safety, and Practicality
Weight Loss Results: Real Numbers from Trials
ScienceDirect publications show amycretin producing twenty-four percent mean weight reduction after thirty-six weeks. Cagrilintide plus semaglutide achieved roughly twenty percent loss over sixty-eight weeks in REDEFINE cohorts. BELIEVE data combining semaglutide with bimagrumab removed twenty-two percent body weight while sparing lean tissue. Meta-analysis indicates these dual approaches reduce visceral fat more aggressively than monotherapies. Such efficacy paves the path toward personalized regimens guided by AI dosing logic.
Side-Effect Profiles and Patient Tolerability
Gastrointestinal events remain the most common complaints, especially nausea during titration phases. Trial investigators report symptoms usually peak within three weeks, then fade as dosing stabilizes. Incidence mirrors standalone GLP-1 data, indicating amylin does not exacerbate intolerance. Serious adverse events remain rare, and no fatal outcomes surfaced during published studies. Vitamin injections may support energy and recovery during initial adjustments.
Integrating These Advances Into Clinical Practice
Endocrinologists already evaluate patient eligibility based on BMI, comorbidity, and previous medication response. Early adopters prefer combination therapy when appetite control remains difficult on GLP-1 monotherapy. Clinics integrate dietitians to help patients adjust meal size, preventing unnecessary hypocaloric fatigue. Physicians schedule monthly visits during titration, then shift to quarterly reviews once targets stabilize. Our rejuvenation and healing programs assist post-weight-loss recovery and long-term success. Questions about this topic? We can help! Give us a call at 239-355-3294 .
FAQ: Smart Weight Loss with Dual Pathway Therapies
What makes dual-pathway therapy more effective than GLP-1 alone?
Dual agents attack appetite from two hormonal angles, limiting compensatory hunger mechanisms. Clinical trials reveal consistently greater fat loss without extra muscle depletion.
How safe is combining GLP-1 with amylin—any added risks?
Published safety data show gastrointestinal effects similar to GLP-1 monotherapy. Serious adverse events remain rare, yet physicians still monitor renal and pancreatic markers.
When might the oral amycretin become available for patients?
Phase 3 trials begin in early 2026. If successful, approvals could arrive in late 2028 or early 2029.
Can AI dosing models really replace human dose adjustments?
AI enhances clinical precision but does not replace medical oversight. Doctors still set parameters and review outcomes.
5 Practical Tips for Patients and Clinicians
- Track daily hunger, energy, and mood using a simple app, then share trends during follow-ups.
- Titrate slowly by increasing dose only when nausea resolves for three consecutive days.
- Eat protein-rich snacks before dose administration to buffer gastric discomfort.
- Perform resistance training twice weekly to protect muscle during rapid fat reduction.
- Call the clinic immediately if persistent vomiting or severe dizziness occurs.
Looking Ahead: The Future of AI-Personalized Obesity Treatment
Recent AI research predicts full integration of hormone dosing with wearable data by the end of the decade. Telehealth platforms will deliver real-time dose adjustments based on behavior and biometrics. Stakeholders expect AI-guided co-agonists to become mainstream once large-scale trials confirm cost-effectiveness. Regulators will demand real-world data proving these platforms sustain fat loss safely across populations.
Medical review: Reviewed by Dr. Keith Lafferty MD, Fort Myers on August 26, 2025. Fact-checked against government and academic sources; see in-text citations. This page follows our Medical Review & Sourcing Policy and undergoes updates at least every six months.